
In obstetrics, DIC is mostly a consequence of either of these: It’s a rare complication in pregnancy overall, but common in the setting of certain pregnancy complications, like amniotic fluid embolism and placental abruption. It’s characterised by both thrombosis and haemorrhage. DIC Definitionĭisseminated intravascular coagulation (DIC) is what occurs when something causes an uncontrolled activation of coagulation and fibrinolysis. The lecture mentions giving dexamethasone routinely in all cases of HELLP, but this is not recommended according to UpToDate and current guidelines. Gestational age is administer RDS prophylaxis (dexa- or betamethasone) -> initiate delivery 1 – 2 days later.Class I – Platelet count 34 weeks -> delivery is initiated.The severity is classified according to the Mississippi classification and is based on the degree of thrombocytopaenia. The liver enzymes are elevated due to liver damage, but the pathomechanism which leads to haemolysis, liver injury, and thrombocytopaenia is not well known.


However, the outcome is usually good for both the mother and the foetus. It can lead to DIC, liver failure, acute kidney injury, ARDS, and even death. It’s one of the hypertensive pregnancy disorders (together with preeclampsia and eclampsia). HELLP syndrome is an abbreviation of Haemolysis, Elevated Liver enzymes, and Low Platelet count. HELLP syndrome Definition and epidemiology Survivors often sustain permanent neurological injury due to cerebral hypoxia. The maternal death rate is high, approximately 20%. If the child has not yet been delivered, C-section should be initiated urgently. Failing organ systems must be supported, and the patient may require fluids, ventilation, vasopressors, dialysis, transfusion, ECMO, etc. TreatmentĪll cases require emergency intensive care and stabilisation. Clinical investigations must be performed while the patient is treated. The diagnosis is clinical and made when other differential diagnoses (PE, anaphylaxis, sepsis, AMI, haemorrhagic shock, air embolism, eclampsia, etc.) are excluded. Hypotension, dyspnoea, cyanosis occurs initially, with DIC, acute heart failure, haemorrhage, and ARDS following. The clinical presentation of AFE occurs abruptly, catastrophically, and progresses rapidly. Activation of coagulation factors and platelets causes DIC, potentially causing multi organ failure. Pulmonary pressures increase, causing RV and subsequently LV failure, as well as pulmonary oedema and respiratory failure.
#DIC AMNIOTIC FLUID EMBOLISM FREE#
However, how this leads to the clinical syndrome is not well known, but it is likely that foetal components activate hormonal and immunological processes which free vasoactive and procoagulant substances.

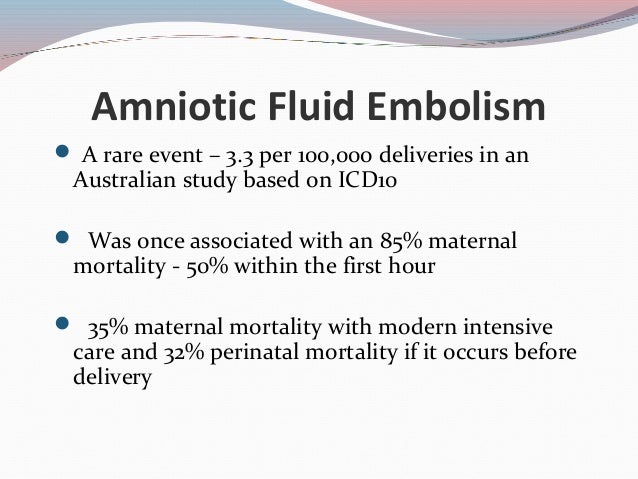
PathomechanismĪmniotic fluid enters the maternal circulation through a breach in the maternal/foetal circulation interface. Complicated labour, placental abruption, and preeclampsia may be risk factors. As such, it’s difficult to predict who will develop the complication. Thankfully, it is rare (1 – 10 per 100 000 deliveries). It occurs during labour or within 30 minutes postpartum. It causes a systemic inflammatory response syndrome (SIRS)-like syndrome and is an obstetrical emergency which is often lethal. Last updated on Januat 19:05 Amniotic fluid embolism Definition and epidemiologyĪmniotic fluid embolism (AFE) refers to the entry of amniotic fluid (which contains foetal cells or hair) into the maternal circulation, which then embolise.


 0 kommentar(er)
0 kommentar(er)
